In Victorian times around 15% of children died before reaching their fifth birthday – often because of bacterial infections as complications to childhood viral diseases, like chicken pox, measles and whooping cough. Now we take for granted that our GP will be able to prescribe antibacterial drugs that will protect us against the various bacteria that assault us. Until the 1970s, the prevalence of deaths from the effects of atherosclerosis ensured that cancer and the various forms of senile dementia were statistically less important. This has all changed thanks to the availability of new drugs for preventing heart attack and stroke, such as the β-blockers and statins. But are we being too complacent?
The burgeoning press reports of deaths from MRSA bacteria and from the new scourge of hospitals – Clostridium difficile – are forceful reminders that new antibacterial drugs are urgently needed. And the unknown effects of long-term use of statins, together with the likely link between the current ‘epidemic’ of obesity and an increased incidence of heart disease, are new factors that may shake our complacency.
Antibiotics: winners or losers?
The triumph of the penicillins in the 1940s was short-lived since the bacteria soon mutated to produce enzymes that destroyed the antibiotics, or induced cellular mechanisms that denied entry to the drugs. Since the penicillins are semi-synthetic, the basic skeleton produced through fermentation technology could be modified to produce new antibiotics with better absorption properties and spectra of activities.
Of the hundreds of antibiotics produced, Beechams’ amoxicillin remains one of the most used, not only for its efficacy but also because it is cheap. It is, however, sensitive to the destructive effects of β-lactamases, produced by some bacteria, which break open the key β-lactam ring. The isolation, by Beechams chemists in 1977, of the natural product clavulanic acid, from Streptomyces clavuligerus, which inhibits these enzymes, was a seminal discovery. This led to the introduction of the drug combination amoxicillin and clavulanic acid (Augmentin), which is still widely prescribed for potentially life-threatening respiratory and urinary infections caused mainly by gram-positive bacteria. Over the years vast numbers of novel β-lactam antibiotics have been synthesised, though most of these – the cephalosporins, carbapenems and monobactams – are only used in hospitals, owing to their expense or the need for intravenous infusion.
The search for antibacterial compounds from the Streptomyces was richly rewarded with the discovery of the tetracyclines and macrolide antibiotics, with doxycycline and erythromycin/clarithromycin currently the most prescribed members of these two families, especially for respiratory infections. Like the β-lactam antibiotics, these have structures produced mainly by the moulds with only modest chemical modification in the laboratory. So the wholly synthetic fluoroquinolones, such as ciprofloxacin and norfloxacin, which act by inhibiting bacterial DNA gyrase enzymes essential for bacterial replication, were another major discovery of the 1970s. They are particularly useful because they are active against urinary infections caused by gram-negative bacteria.
Despite the efficacy and relative cheapness of all these antibacterials, the increasing incidence of drug-resistant bacteria means that a patient with pneumonia or other life-threatening bacterial infections will usually be treated with ever more complex and expensive antibacterials. These are aimed at clearing the lungs of infection but will inevitably destroy more than 95% of the normal gut bacterial flora, leaving the way open for the opportunistic anaerobic bacterium Clostridium difficile to initiate a potentially, life-threatening infection.
The antibacterials vancomycin, from Streptomyces orientalis (Lilly, 1955) and the synthetic metronidazole (Rhone-Polenc, 1960) are usually effective against C. difficile. In addition, all the time that we continue to use vast amounts of antibiotics in agriculture and husbandry, the bacteria will have every opportunity to encounter them and mutate to produce resistant strains. This is presumably what has happened in the recent E. coli outbreak in Germany. So 70 years of R&D with antibacterials has left us only marginally ahead of the bacteria.
Heart problems
While antibiotics revolutionised the treatment of acute illness caused by bacteria, the β-blockers, ACE – angiotensin converting enzyme – inhibitors and, more recently, the statins have had a similar impact on the chronic effects of atherosclerosis, the clogging up of arteries by fatty deposits. The involvement of cholesterol in the development of atherosclerosis was proved by the US Framingham study in 1957, and the deposition of fat and cholesterol-rich deposits in arteries was recognised as a major risk factor for narrowing of the arteries, leading to heart attack and stroke.
Regulation of serum cholesterol levels by statins had to wait until the late-1980s, but the control of blood pressure by use of β-blockers, from the 1960s, and ACE inhibitors, from the 1980s, had a huge impact on the death rate from cardiovascular disease. Prolonged elevation of blood pressure – hypertension – not only damages the arterial wall but also increases the risk of heart attack and stroke.
The β-blockers, discovered by Sir James Black and his team at ICI, selectively block the effects of adrenaline and noradrenaline on heart muscle, and this decreases blood pressure by lowering cardiac output but improving cardiac efficiency. Examples of β-blockers include propranolol or atenolol. Alternatively, the ACE, inhibitors, like captopril (Squibb) and enalapril (Merck), inhibit the conversion of the hormone precursor angiotensin I into angiotensin II – a peptide hormone that normally increases blood pressure by constricting the arteries. A combination of ACE inhibitor and β-blocker has been the treatment of choice for hypertension for the past three decades.
The proven link between elevated serum cholesterol levels and cardiovascular disease coincided with elucidation of the biosynthethic pathway of mevalonic acid to cholesterol, a process that occurs mainly in the liver. So it was natural that the pharmaceutical industry should search for natural inhibitors of this process. Two fungal natural products were soon discovered – mevastatin in 1976 and lovastatin in 1979 – and this led ultimately to the introduction of lovastatin (Mevacor) in 1987 as the first clinically approved statin.
In the ensuing 25 years, most of the larger pharmaceutical companies have developed their own statins, and of these Lipitor (Pfizer), Zocor (Merck) and Crestor (Astra-Zeneca) have been the most successful. Patients typically achieve a 25% reduction in serum cholesterol levels and up to 35% reduction in LDL or ‘bad’ cholesterol, and there is excellent evidence that the use of statins, in conjunction with low dose aspirin, which reduces platelet aggregation; β-blockers; and ACE inhibitors, significantly reduces the incidence of heart attack or stroke for those who have already suffered a first incidence.
However, the jury is still out concerning the preventative effects of this therapy when taken by middle-aged ‘at-risk’ patients. For the pharmaceutical industry this is a fantastic drug regimen since patients may well take these drugs for 30–40 years. For the patient, the expense of the drugs over the same period and the unknown longterm side-effects should not be underestimated.
AIDS and cancer – some success
It is exactly 30 years since the first cases of AIDS were reported. During this period around 60m people have been infected by the human immunodeficiency virus (HIV) and more than 33m have died from AIDS. Yet the successful treatment of the disease provides a powerful example of what can be achieved when chemists and biologists collaborate with almost unlimited access to research funding.

Treatment of HIV positive patients with a combination of these two types of drugs can reduce the amount of HIV to undetectable levels, but this regimen is not curative and the patient must take the drugs indefinitely. This is expensive so most HIV positive people in developing countries do not receive drug treatment. Nonetheless, the rapid discovery of these life-saving drugs was a staggering achievement, though we may not be so lucky next time if the emerging virus can be transmitted by droplet infection, like influenza, rather than by the relatively inefficient venereal route. The recent, so far, unfounded threat of pandemic swine flu demonstrated the difficult and expensive choices – vaccination and/or drug provision, and for which sections of the population – facing governments when a new virus appears.
Until the mid-1970s, a diagnosis of cancer was usually a death sentence for the patient. Since then, spectacular advances in surgery, radiotherapy and chemotherapy have provided the means of complete cure for certain cancers, and greatly extended periods of remission for other cancers.
Several relatively rare cancers like Hodgkins lymphoma, testicular teratoma and childhood leukaemia can usually be cured through the use of cocktails containing both synthetic and natural product-based drugs. In both breast and prostatic cancers, the successful use of sex hormone-suppressing drugs, like tamoxifen and gosserelin, respectively, arose from the recognition that growth of these cancers is usually hormone-dependent. For most other cancers and for advanced metastatic cancer, chemotherapy has only been partially successful. Natural productderived drugs, like taxol, the vinca alkaloids and doxorubicin, together with the wholly synthetic 5-fluorouracil, carboplatin, cyclophosphamide and cytarabine, can increase survival times and produce cures.

An expensive future
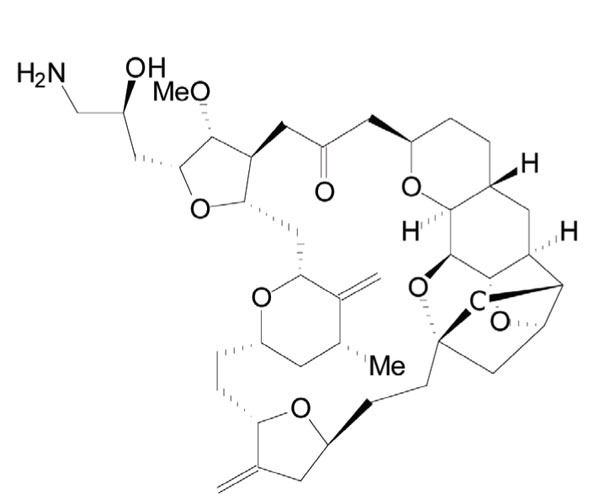
The newer natural product-based drugs are very expensive. Take, for example, the experimental drug Halaven (eribulin), recently approved by the FDA for the treatment of advanced breast cancer, which is a simplified analogue of the sponge metabolite halichondrin B. It took 62 chemical steps to make this compound and the chemists had to locate no fewer than 19 stereocentres during their synthesis. While this demonstrates the power of modern synthetic chemistry, one can only guess at the likely price of this drug if it receives full clinical approval.
Most pharma companies now employ virtual screening as a computational tool to predict the likelihood that particular sub-structures in compound libraries will interact with a protein or enzyme of interest. Key parameters, such as molecular weight, lipophilicity and likely resistance to metabolism, can be built into the selection process so that only the most promising potential leads are chosen. While this approach will undoubtedly provide small molecule drug candidates, there is a growing interest in the design of novel natural products through genetic manipulation. After all, natural products have been around for a very long time, which implies that their interactions with the components of cells – DNA, enzymes etc – have been deemed acceptable by the evolutionary process.
As the genes involved in natural product biosynthesis are identified, it should be possible to manipulate the pathways of biosynthesis by deliberate mutation of the gene structure – mutagenesis – or by gene shuffling, and thus produce natural products that have never before been biosynthesised. This strategy has already been tried with the gene sequence for erythromycin biosynthesis and novel compounds with antibacterial properties have been obtained. Interesting hybrid structures have also been obtained when parts of the genomes of two different microorganisms have been merged. The possibilities for the creation of new natural products with potentially useful clinical activities are almost limitless, but this research is at an early stage and will be expensive. One thing is certain – most of the cheap life-saving drugs have already been discovered.
John Mann is emeritus professor of chemistry at Queen's University Belfast, UK.





