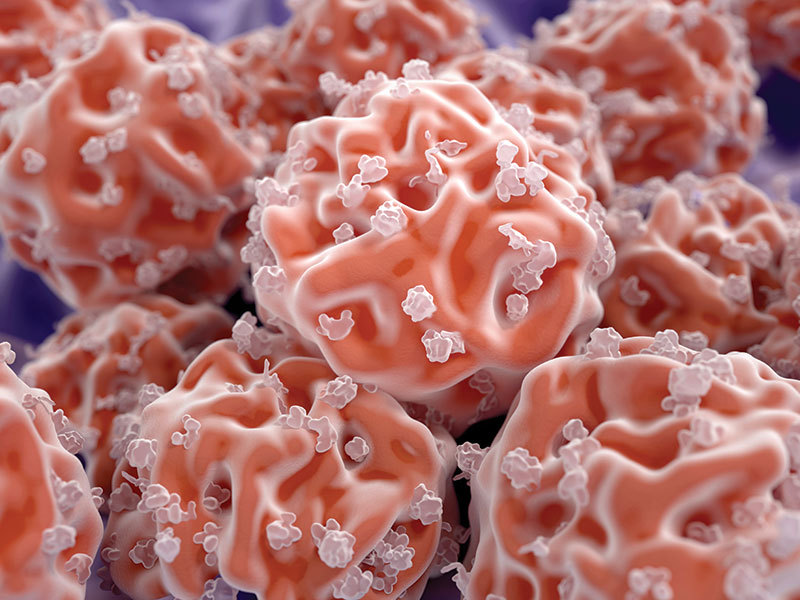
Cartilage has little to no regenerative ability, but synthetic tissues are already in the pipeline that match its properties, Katrina Megget reports
Injuries of articular cartilage – the white, slippery material at the end of bones, cushioning the joints – are common. Osteoarthritis is where bone grinds on bone and follows wear and tear leading to localised cartilage lesions. Studies suggest cartilage lesions occur in between 30% and 60% of people – even without symptoms.
‘The impact that articular cartilage injuries have on peoples’ lives is great,’ says Wayne Gersoff, an advanced orthopaedic and sports medicine specialist in Denver, Colorado, US, and member of the International Cartilage Regeneration and Joint Preservation Society (ICRS). ‘These injuries will cause pain, swelling and decreased function not only for recreational activities but also for activities of daily living.’
Cartilage, a tough and flexible connective tissue, comprises 65-80% water attracted to a mesh of negative charges in a gel-like matrix of proteins including collagens, proteoglycans and non-collagenous proteins. Together, the water and protein matrix create the strong, cushiony environment that protects the bone and allows fluid movement of the joint.
While cartilage is strong and durable, it has little to no regenerative ability in adults once it is damaged or lost. Very few cartilage cells – chondrocytes – actually exist in cartilage, and it has no blood vessels, no nerves and no lymphatic system. Because of its inability to fully regenerate, treating damaged cartilage poses a problem.
With more advanced damage in osteoarthritis, patients can only rely on some form of joint replacement. With less severe forms of injury, there are various treatment options aimed at cartilage repair, such as microfracture, where tiny holes are drilled in the surface of a joint. This stimulates the bone marrow to form the scar tissue-like cartilage called fibrocartilage. This, however, is only a short-term solution as fibrocartilage is mechanically inferior and will break down over time.
A more advanced procedure is osteochondral autologous transplant system (OATS), sometimes called mosaicplasty. This involves grafting plugs of undamaged cartilage onto areas missing cartilage. Donor grafts can also be used. Again, this can have issues over the long-term.
Autologous chondrocyte implantation (ACI) is more advanced still, where chondrocytes are harvested from the joint during surgery, grown in a lab into a new cartilage graft and implanted back into the joint in a second surgical procedure about four weeks later. ACI is considered the current gold standard for regenerating cartilage but requires a licence to culture the cells and is expensive. In the UK, the procedure is not widely available, and the only lab currently licensed to produce these cells is at The Robert Jones and Agnes Hunt (RJAH) Orthopaedic Hospital in Shropshire.
‘At the moment what we have [as treatments] is good but it is limited in how many patients it is available to and we should always be aiming to do better for more of our patients,’ says Paul Jermin, consultant orthopaedic surgeon at RJAH. He says the aim should be to improve current treatments in the earlier stages of damage and prevent damage reaching the osteoarthritic stage and joint replacement. ‘If we are to move forwards, start rationalising our treatments and be more scientific in our approach, further research is imperative – and some excellent research is being done in this area. Ultimately, this is about treating people and trying to improve their symptoms and quality of life.’
Research activity has increased dramatically since 2010, notes Gersoff. Research into new technologies is still in its infancy but he says it is an exciting time for the field. ‘In essence we are in constant search for the holy grail.’
That holy grail could come in the form of synthetic tissue. Artificial tissue made from hyaluronic acid or collagen has already been developed, but researchers at Duke University, US, say they have created the first synthetic material to match the strength, durability and lubricity of natural cartilage. The jelly-like material is 60% water and 40% biocompatible polymers and about the size of a US quarter, but can bear the weight of a 45kg kettlebell without tearing or losing shape.
65%
Cartilage comprises 65-80% water attracted to a mesh of negative charges in a gel-like matrix of proteins including collagens and proteoglycans.
A specialised population of cells in the skeleton of an adult skate possesses the ability to generate new cartilage throughout the animal’s life. Genetically engineering mammalian cells to perform more like skate cells could produce a more stable, permanent cartilage end product.
45kg
The first synthetic material to match the strength, durability and lubricity of natural cartilage is 60% water and 40% biocompatible polymers. The jelly-like material is about the size of a US quarter but can bear the weight of a 45kg kettlebell without tearing or losing shape.
Technology using protein factors may one day pave the way for ‘like with like’ resurfacing of damaged joints with true cartilage, rather than invasive joint replacement surgery.
This is thanks to the polymers that form two intertwined networks: one more stretchy and the other more rigid with negative charges along its length. The polymers are reinforced by a meshwork of cellulose fibres, which resist pulling and help hold that material together when stretched. Meanwhile, the negative charges along the rigid polymer chains repel each other and stick to water when the gel is squeezed, allowing the material to keep its shape.
The team put the synthetic material through its paces, subjecting it to 100,000 cycles of repeat pulling and rubbed it against natural cartilage a million times. They found that the hydrogel was as wear-resistant as natural cartilage and four times more wear-resistant than synthetic cartilage implants currently regulator-approved for use in the big toe.
‘Many patients are too young to receive a total knee replacement but lack any good options that can allow them to enjoy an active lifestyle. We are designing our implant exactly with these patients in mind,’ says Benjamin Wiley, professor of chemistry at Duke University. ‘Since we are not trying to regrow cartilage but are instead seeking to replace it with a material that mimics cartilage, we can offer patients a solution that does not require them to regrow cartilage in their damaged joint [like current treatments]. We believe our approach can offer reduced recovery times and lower failure rates and is a cost-effective solution.’
The gel has received Breakthrough Designation status from the US FDA and Wiley’s team is carrying out preclinical testing ahead of clinical trials in humans, which they hope to start enrolling for in 2022. He believes the synthetic cartilage could be approved for use as early as 2026.
The flipside of synthetic tissue is using the body’s own cells and substances to promote cartilage regeneration. In ACI treatment, these are cartilage cells. But Jermin notes these may not necessarily be the best cells to produce cartilage. As such, interest is turning to stem cells with their potential to differentiate into different cell types. ‘Stem cells present an interesting problem, and more research is required to determine their potential,’ says Gersoff.
That said, some commercial companies already offer stem cell treatments for cartilage and joint injuries. But injections of stem cells into the joint have not been clearly proven as a regenerative treatment, Gersoff says. It may reduce symptoms due to anti-inflammatory action but may not necessarily repair cartilage. Jermin agrees, adding stem cells are complex, having to form into the right tissue in the right place and function appropriately, and evidence of regeneration is thin on the ground. Some studies show promising results, but Jermin says the vast majority of injections performed have no published outcomes of how well people do from the treatment.
Commercial companies have jumped on the term stem cell and have looked to monetise it. We as a medical community need to be doing better here, and further, well-conducted research is essential to looking at the potential benefits for treating people with cartilage damage.’
For his part, Jermin is involved in a UK trial, led by Peter Gallacher, consultant orthopaedic knee surgeon at RJAH, which is evaluating the safety and efficacy of cartilage cells, compared with bone marrow stem cells in treating cartilage lesions of the knee. The ASCOT Trial (Autologous Stem Cells, Chondrocytes or the two), which is part funded by the UK charity Versus Arthritis, aims to see if bone marrow stem cells (which can develop into bone or cartilage) will be able to repair the damage to joints better than cartilage cells or whether a combination of the two cell types is better. The results of this trial could be used to improve the ACI procedure.
‘We hope that we can find a source of cells that work very well at producing cartilage so we can mass produce them – thereby making the ACI procedure more widely available in the UK – and so that we have an off-the-shelf source of cells, ready to go for anyone who may benefit from the procedure,’ says Jermin, who is also working on new surgical methods to use keyhole surgery for both ACI surgery stages, which would replace the second more invasive operation. Recruitment for the ASCOT trial is still open, with final results expected in a couple of years.
Understanding how cartilage is formed could provide answers on how to enhance cartilage regeneration. At the University of Cambridge, UK, a team is working backwards, studying a model for cartilage growth and repair that has not been explored before. ‘In mammals, cartilage is largely an embryonic tissue and is almost entirely replaced by bone during development and growth,’ explains Andrew Gillis from the department of zoology. ‘Cartilaginous fishes, such as sharks, skates and rays, have a skeleton that remains cartilaginous throughout life – and what’s more, they continue to grow this skeleton throughout adulthood.’
The team discovered a specialised population of cells in the skeleton of the adult skate that possesses this ability to generate new cartilage throughout the animal’s life. ‘What we have found is that skates have a tissue layer called a perichondrium that wraps around their cartilaginous skeleton, and they have cartilage progenitor cells embedded within the layer.’
Now Gillis wants to discover the cellular and molecular mechanisms skates use to achieve continuous cartilage regeneration. He says humans do not have a comparable cell type in or around their articular cartilage so it would be unlikely to mimic the activity in humans. ‘What we do hope is that we can discover the molecular differences between developing cartilage cells in skate and mammals. Then we hope to use those differences to edit mammalian cells so they can perform more like skate cells during in vitro cartilage engineering, ultimately producing a more stable, permanent cartilage end product.’
The team is using high throughput sequencing methods to discover all the genes expressed in skate cartilage cells and in the progenitor cells, while also looking at non-coding regions of the genome that might control gene expression.
We are not trying to regrow cartilage but are instead seeking to replace it with a material that mimics cartilage. We believe our approach can offer reduced recovery times and lower failure rates and is a cost-effective solution.
Benjamin Wiley professor of chemistry, Duke University, US
Meanwhile, researchers at Stanford University School of Medicine, US, are looking at a similar concept of engineering cartilage regeneration. According to Charles Chan, assistant professor of surgery, who studies regenerative medicine at Stanford, research shows that when bone develops, cells have to first go through a cartilage stage before turning into bone. The team aimed to stop the process at the cartilage stage.
Using skeletal stem cells, which form bone, cartilage and fibrous tendon-like cells, and are activated during microfracture treatment, the team used the protein factor bone morphogenetic protein 2 (BMP2) with a vascular endothelial growth factor inhibitor to steer the growth of the stem cells to induce true cartilage regeneration in mouse joints. ‘What we ended up with was cartilage that is made up of the same sort of cells as natural cartilage with comparable mechanical properties, unlike the fibrocartilage that we usually get [during microfracture]. It also restored mobility to osteoarthritic mice and significantly reduced their pain,’ says Chan.
The team also transferred human tissue into mice and were able to replicate the results. The next step is to conduct large animal studies, with the therapy entering clinical trials within the next 18 months, Chan says. ‘Our technology, once fully translated for human clinical use, would provide a way for ‘like with like’ resurfacing of damaged joints with true cartilage, rather than invasive joint replacement surgery.’
Looking at the role molecules can play in cartilage regeneration, like Chan’s use of protein factors, could also make strides in the treatment of cartilage injuries. At Queen Mary University of London, researchers are investigating the large proteoglycan agrin in mice and sheep, which they found can activate dormant stem cells in cartilage and instruct them to repair an injury. Meanwhile, a team at the University of Southern California, US, has produced a clinical analogue of the molecule RCGD423 (Regulator of Cartilage Growth and Differentiation) called CX-011. The molecule appears to enhance regeneration by communicating with the glycoprotein 130 (GP130) receptor. It will enter clinical trials in 2022.
Gersoff describes the future as both exciting and promising. He expects dramatic improvements in treatments, success rates and cost. ‘With research, the next great threshold will be in the use of orthobiologics – such as stem cells – either as a direct treatment for articular cartilage injuries or as an adjunct to improve the results of established surgical techniques. I’m not sure when we will achieve that holy grail but hopefully we will come close in the next three to five years.’
None of this will come before time. Nearly half of American adults will develop knee osteoarthritis in their lifetime, according to the American Academy of Orthopaedic Surgeons (AAOS). Around one million knee and hip operations are performed annually in the US and AAOS predicts knee replacement surgeries in the US alone will grow 673% to 3.5m procedures/year by 2030.
Images: Top - RODRIGO FRISCIONE/CULTURA/SCIENCE PHOTO LIBRARY | In-page - JUAN GAERTNER/SCIENCE PHOTO LIBRARY